I’m on a journey, one I’ve never been on before. It’s not exactly a “magical mystery tour”, for I know the destination — the terminus — and while I can guess at some of the intermediate stops, I can’t be certain of them. I imagine I’m in a steam train, a slow train which stops everywhere, though sometimes it might be an express. I don’t know how long this journey will take, though my fare is a single rather than a season ticket or even a day return. At least I don’t have Michael Portillo with an antique Bradshaw accompanying me. Confused? Relax, sit back, and let me tell you a story.
This all began about three years ago. Actually, it didn’t begin then, but a couple of years before that, or perhaps even longer than that. But I only became aware of the journey three years ago.
I noticed a swollen right shin and calf, and went to the GP. He got very excited, trying to tell me I had a deep venous thrombosis (DVT), a blood clot in the leg. I didn’t think anything of the sort. He arranged for me to have a scan of the leg in Craigavon — there is a very fast-track service for this; and I had to inject myself with blood-thinners for a couple of days. He also did a series of blood tests, and I got the results the next day.
I had to wait over the weekend for the ultrasound scan; it’s just rubbing the machine along the leg. As I thought, there wasn’t any clot, but the eagle-eyed sonographer saw a gland in the groin which pretty well settled the diagnosis. The blood tests included a prostatic specific antigen (PSA), and this was very elevated, strongly suggestive of prostate cancer. The lymph gland in the groin was visible because it was enlarged as the cancer had spread to it; and the swelling in the leg was because the lymphatic channels were blocked there so that excess tissue fluid couldn’t drain away.
Actually, the GP sent me to the A&E in Craigavon and from there I went for the scan. After it, I returned to the A&E and discussed the results with the doctor; she went off to discuss them with a radiologist, and returned soon after to say I was going to have a whole-body CT and a bone scan.
I’m sure most of you know what a CT involves; I had it in South Tyrone. For the bone scan (in Craigavon) I was injected with Technetium, an artificial radio-isotope with a very short life. Technetium is made in the EU. There’s a bit of a wait for the isotope to be taken up by the bones, then it’s just lying flat and motionless for a while. Prostatic cancer very typically spreads to glands and bones.
The CT showed glands in the pelvis, abdomen, and chest; the bone scan showed mets (metastases, secondary deposits of cancer) in the bones in my back and around the left shoulder, and a few elsewhere; nothing really surprising about this. The CT threw up a few oddities — mega-sized adrenal glands, a few extra ureters, that sort of thing — so I then had an MRI (magnetic resonance imaging) scan for clarification. I’ve always thought it odd that they never worry about the great hunk of steel in my right shoulder — a prosthesis after a bad break about 15 years ago; it was only later I discovered that there are several types of stainless steel and not all of them are magnetic. That’s why some of our nice stainless-steel pots wouldn’t work on the new induction hob. The MRI didn’t show anything worrying.
After this, the train took a detour for a while before anything more happened. That was a visit to the Urology out patients in Craigavon. It’s a “one stop shop” where a full clinical assessment takes place. It ends up with a series of ultrasound guided biopsies of the prostate, done per rectum; this is as uncivilised as it sounds, though doesn’t take long. These nibbles, over twenty in my case, go off to the pathologist for microscopic examination and an assessment of the degree of malignancy or badness. This is called a Gleason Score, and is based firstly on how bad the most common cells look, and secondly on how the “non-dominant” cells look. My score was 4 + 4 = 8 which is moderately bad (or good rather like half-full or half-empty).
After this, the urologists, radiologists, pathologists, and oncologists meet up in a “multi-disciplinary team” to chew the fat and consider what happens next. I was reviewed soon after this, told the (unsurprising) results, and the treatment plan. This was a depôt injection of Decapeptyl given then and there — other varieties are available; the effect lasts three months. It is a testosterone blocker, which sounds fancy, but it’s really a form of chemical castration. Prostatic cancers very typically are “driven” by testosterone, and removal of the hormone will slow or even stop progression of the disease. Alas, the side effects include a menopause complete with hot flushes and sweats. I’m still on Decapeptyl which is made in France, and was difficult for the pharmacist to source recently; not the joy of Brexit, surely?
Prostate cancer is a funny-peculiar disease. The only clear risk factor is increasing age, and there’s not much any of us can do to avoid this. It is really very common — almost ubiquitous — in advanced old age. At one extreme it can remain limited to the gland, with no spread and can be surgically removed or destroyed by radiotherapy. Sometimes, it seems to be “indolent” and just remains in the gland and doesn’t do much, and indeed may not actually need any treatment. At other times it’s much nastier — hence the Gleason scoring, and the scans to work out a plan of campaign.
I was then reviewed every few months in the Cancer Centre at the City Hospital; my PSA fell markedly with the Decapeptyl, but later showed a very gentle rise, as to be expected. I had occasional check CTs — I’m losing count of how many I’ve had, but so far, I don’t glow in the dark. After a year or so of this, I was advised radiotherapy to the prostate itself; this apparently helps to control the metastatic disease elsewhere. I though this distinctly odd, as it sounded like gravity — “spooky action at a distance”.
The swelling in the right leg had become very tense and unpleasant, with a “violaceous” discolouration over the shin. With the treatment, it gradually improved. I went off on a branch line to the expert lymphoedema physiotherapist in Portadown Health Centre. I tried the Flowtron treatment, a sort of mechanised massage, but wasn’t impressed. Now I have the lower leg in elastic strapping, and it’s comfy enough.
I had to be “measured up” at my first radiotherapy attendance; this is done using a CT to exactly define where the prostate is, and I got three marker tattoos for the exact alignment of the radiotherapy machine. I’d never expected I’d be buried in a Jewish cemetery, but this is now impossible.
The radiotherapy is given not as one mega-dose but as twenty “fractions” spread over four weeks so that there isn’t major damage to neighbouring structures and the skin. I just had to lie flat and get aligned with the machine. The machine emits a cone of radiotherapy, and this is focused at the area to be treated. The beam is rotated in an arc around the prostate, to maximise the dose there, and to minimise the dose elsewhere. My only problem was getting off the table — I had to lie quite flat — and overusing my left shoulder it later became frozen and painful.
While the train journey to the end of 2019 was unexciting, 2020 saw me off on side-excursions I could well have done without. The pain at the left shoulder settled pretty much, and movements slowly returned.
Then one evening, sitting looking at the computer monitor to see what you lot were up to on Slugger, with my left arm resting on the table, I got a sudden, severe pain in my left chest; I didn’t at first know what it was. Wrong place for a heart attack, and when it eased a bit, it was clear that I’d had a “spontaneous” fracture of the left clavicle (collar bone); this was of course full of mets. This was confirmed by x-ray at the next station on this branch line, the Minor Injury Unit at South Tyrone Hospital, and I was put in a Polysling. If you ever have anything similar, insist on this type of sling, it’s so much more comfortable that a simple sling (a mitella). I saw the orthopod at the Fracture Clinic in Craigavon; he thought I should have a plate; I didn’t think that, and in fact, the fracture healed, and at a further review I was discharged. There’s an impressive lump there, a mixture of the mets and bone healing, I guess. Luckily, I don’t wear strapless tops.
There were two further deviations on the branch line; I seem to have sleep apnoea — periods during sleep when you stop breathing. I’d been getting early morning headaches, a very typical symptom. I couldn’t get the proper tests for this, because the appropriate staff had been seconded to Covid care, but I was able to get a CPAP (continuous positive airway pressure) machine to use at night; the headaches have gone.
The next problem was severe shortness of breath so I could barely walk across a room. Much “routine” diagnostic work had been put on hold because of Covid, but I was advised to go to the A&E in Craigavon. Actually, there are now two A&Es, one for people suspected of having Covid, and another for the other problems. This latter is in what was the canteen, and there is instead a marquee now at the front car park. A chest x-ray showed I had a large left pleural effusion (fluid on the lung); no wonder I couldn’t expand the lung.
Arrangements were made for me to have this drained at another stop down the line, at Daisy Hill Hospital. There, I was stabbed in the back — it wasn’t sore — and about 1.2 litres (over two pints) of fluid removed. (I’m quite sure if my former colleagues had known about the backstabbing, there would have been quite the queue.) This helped the breathing a lot, and follow up x-rays showed that the remaining fluid was gone. While there were some hazy shadowy things seen in the lungs, it was never clear what had caused this; it wasn’t caused by the cancer.
Meanwhile, back on the main-line as it were, I had another check-up in Craigavon, in the Mandeville Unit. I was “heighted” and was horrified to discover I’d lost 8 cms because of the collapsed bones in my back. With the Decapeptyl gradually losing its edge, something that happens after a year or eighteen months or so, I was started on Abiraterone, a “second-line” treatment. This can only be prescribed by a hospital consultant, and is given out by the pharmacy there. It’s a sort of general steroid blocker, so is accompanied by prednisolone, a synthetic steroid, to obviate unwanted effects.
Things were largely back on the main line after this, though I did get a tiresome cough which produced gallons of sputum. Oddly, a single dose of Benylin cough mixture turned this off like turning off a tap.
More recently, I had several episodes of being woken from sleep by very severe pain in the blade of the left scapula (shoulder blade). I couldn’t get any comfortable position, and the pills I took to try to control the pain only made me puke. The scans previously did show lots of mets in and around this area.
At a recent check-up, the Abiraterone was stopped allegedly because the PSA was gradually rising; like other treatments, it gradually loses its effectiveness. Another reason for stopping it was that it’s “expensive” — it’s about £1,500 a month. I wasn’t impressed by this reason. I’ve been kept on prednisolone.
It was agreed that I should have radiotherapy for the shoulder pain. This involved getting measured up and a further set of tattoos, and on a second visit, a blast from behind and from the front. This is a typical way to manage or palliate the pain from bony mets.
I also got a home visit from the GP, such a rarity these days and perhaps a sign that things are returning to “normal”. He’s put me on an appropriate dose of MST; this is a long-acting form of morphine. It’s tablets, taken twice a day. If the dose isn’t quite enough, if there is “breakthrough” pain, I also have Oramorph. This is short acting, over four hours or so. I’ve not really needed this so far, but if I have to take it frequently it means the dose of MST should be increased. Interestingly, MST is taken whether you have symptoms or not, to keep on top of things — this is a cardinal feature of palliation. I’ll become a junkie, but so what, it doesn’t matter.
I also got a powder inhaler for the cough and sputum, and so far, it’s very effective. I’m waiting for a follow up appointment (somewhere!) to see if there’s any diagnosis.
It’s time for a little diversion into a siding, time for a pause. When Swiss trains are reaching the end of the line, the announcement tells you that you are arriving at the Endstation, and you must disembark. You know as well as I do what the Endstation is; it’s journey’s end, a journey that we must all make. There are things to do before the Endstation.
You must make a Will; making it won’t have any influence on your personal future, to think so is a ludicrous superstition. But making a Will makes things so much easier for your family. A solicitor will draw one up, often for free or for a very small charge. It’s important to keep your Will up to date; if circumstances change, think about changing your Will to incorporate the changes. Think about your Executors, the people who have to sort things, to deal with the legal bureaucracy. A solicitor is often best placed for this, and you can ask a family member to “assist” if you like. If leaving personal bequests, please make them unconditional.
If the Endstation is visible, even if only on the horizon, I suggest you and your family talk to an undertaker. They are very helpful people and will deal with much of the paperwork. It’s your funeral — quite literally — and the undertaker will listen to your ideas and help with your choices. You are going to be paying for the funeral; it may be possible to pay in instalments in advance, for funerals can be surprisingly expensive. The average cost of a cremation in the UK is said to be nearly £4,000 and for a burial it’s nearly £5,000. (I’m a skinflint, I have no intention of paying that much.) Advance planning like this means so much less hassle for your family. If you have the time, think about simplifying your affairs as much as possible; and take advice about any tax implications. For example, if you and your partner are the “joint owners” of a house, your share automatically passes to the partner on your death; you cannot change this in your Will. You could consider becoming “tenants in common”, each having a share; you can dispose of your share in your Will as you please; it’s also a potential way of reducing “death duties” in the future. This is the sort of thing that we all need advice about.
And while we’re here, there are all sorts of support services available. I have a carer who comes several times a week to help with what’s quaintly called “personal hygiene”, which is drying me off after a shower, and helping to get me dressed. One of the kids put up grab handles at the shower and the loo, and these are really necessary now. The District Nurse comes to take bloods for the PSA before consultations with the oncologist, and to give me the Decapeptyl injection. And they call in between times just to keep an eye on me.
Just before we leave this rather gloomy siding, I’m sure you realise that I haven’t always felt as well as I do now. But the aches etc are in abeyance for now; it does take some professional input to sort things.
I notice too a gradual downhill progression in my abilities. I have carers and minders to help with all the things I can no longer do. This loss of independence is something I find disturbing, though I can’t do anything for it. And with that is the feeling that I might be getting to be a burden on some family members, and that’s something I certainly don’t want.
I see that Michael has filched some fuel from the “fine clamp of turf in the bog there”, some of you are “gathering sticks”, and the fire is going well again. Just before we leave this dismal place, recall that I said that prostate cancer was a funny-peculiar disease. This is seen in the survival statistics. Most cancers are found at an early stage and the 5-year survival rate is nearly 100%. While overall the five- and ten-year survival rates are about 98% — I find these statistics as impressive as they are encouraging — the picture isn’t nearly so rosy for those with advanced disease, when the five-year survival is about 30%. I feel as if I’m going into extra-time at present. And the answer to your question is, “How long is a piece of string?”
Back out in the open, things have brightened up a lot; we’re just puffing gently along, just as I like it. I haven’t always felt so well — sometimes I felt so rotten that I could contemplate a trip to Dignitas in Switzerland, the place that does “assisted dying”. But with help from the professionals, I feel “good” right now, better than I’ve felt for quite some time.
Things have changed a lot since I was a lad. Then having cancer was shameful, a secret to be kept hidden. People talked about “shadows” on x-rays, and there was often the feeling that the patient should be spared the diagnosis; he or she should be kept in the dark, while the relatives did the worrying. This is nonsense today and was nonsense then. The patient is the one with the problem, the patient should be properly (and kindly) told what’s going on, what treatment can be offered, and what to expect. In other words, to be treated humanely just as with any other with a serious disease: cancer is only one disease among so many.
Talking about professionals; the problem, as you all know, isn’t what they do, it’s getting to them, a problem made much worse by Covid last year. Once I got into the system, I was so well treated — even if I’m an argumentative old git — and listened to, and what could be done was discussed with me, rather than me being told. Likewise, the District Nurses, radiographers and carers have all been so good; I’d like to leave this as a mark of my appreciation for their efforts.
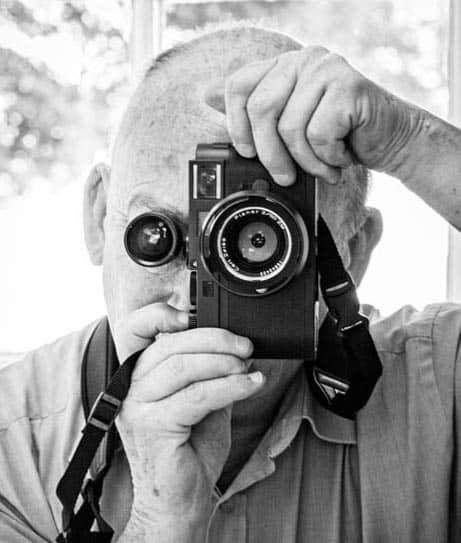
Meanwhile, as I trundle gently off towards the far-distant Endstation, don’t think I’ve gone away. Like the Editor of the Skibbereen Eagle, I still have my eye on yous, and I’m quite compos mentis enough to see what you are up to at times.
My thanks to Claire Mitchell for her Critical Reading.
Robert Campbell is a retired surgeon.
Discover more from Slugger O'Toole
Subscribe to get the latest posts to your email.
